Tissue-Air Ratio (TAR) calculation with MCNP
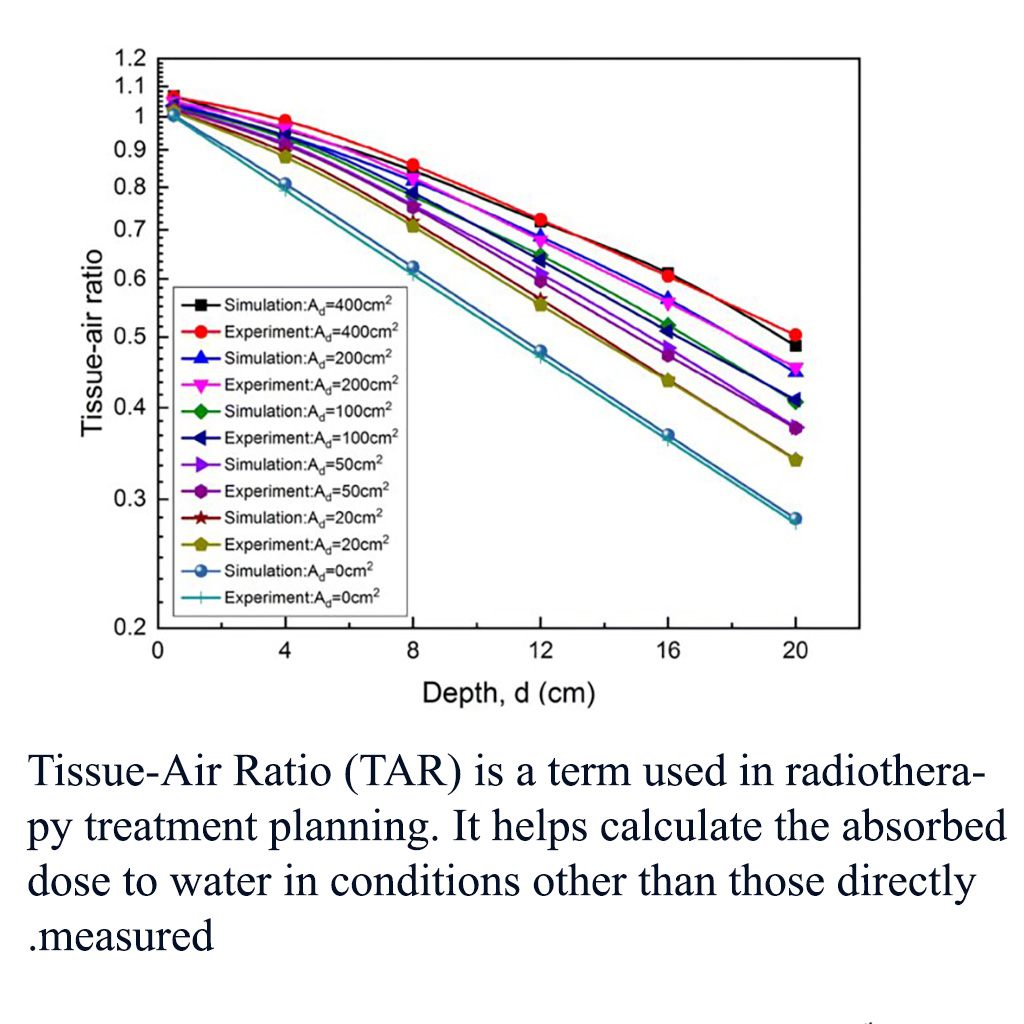
Tissue-Air Ratio (TAR) is a term used in radiotherapy treatment planning. It helps calculate the absorbed dose to water in conditions other than those directly measured.
Table of Contents
Here's a brief overview:
Definition
TAR is the ratio of the dose to water at a given depth to the dose in air measured with a buildup cap. Mathematically, it is expressed as:
TAR=D(f,z)/D(f,0)
where D(f,z) is the dose at a given depth z and distance focus-detector f; and D(f,0)is the dose in air (z=0).
Key Points
- Increases with Beam Energy: TAR increases with increasing beam energy because higher energy radiation is more penetrating.
- Decreases with Depth: TAR decreases with depth due to attenuation.
- Increases with Field Size: TAR increases with field size due to increased scatter contribution.
Applications
TAR is used in dosimetry to ensure accurate dose calculations in radiotherapy treatments
Detailed Calculation
- Reference Conditions:
- Depth (d): The depth at which the dose is being measured in tissue.
- Source to Surface Distance (SSD): The distance from the radiation source to the surface of the patient.
- Field Size: The size of the radiation field at the surface.
- Equation:
TAR=D(d)/D(0)
- D(d): Dose at a given depth dd in tissue.
- D(0): Dose at a reference depth (usually in air).
Factors Affecting TAR
- Beam Quality: Higher energy beams penetrate more deeply and thus have higher TAR values at greater depths.
- Field Size: Larger field sizes increase TAR due to more scattered radiation contributing to the dose.
- Depth: As depth increases, TAR generally decreases because of the attenuation of the beam in tissue.
Importance in Dosimetry
- Treatment Planning: TAR is crucial for accurate dose calculations in treatment planning systems (TPS). It helps ensure that the prescribed dose is delivered to the target tissue while minimizing the dose to surrounding healthy tissue.
- Verification and Quality Assurance: TAR is used in quality assurance procedures to verify the accuracy of treatment delivery.
Practical Applications
- Manual Dose Calculations: Before advanced TPS, physicists used TAR tables for manual dose calculations.
- Verification of TPS: Even with modern TPS, physicists may use TAR for independent verification of dose calculations.
Modern Relevance
While modern treatment planning systems use more sophisticated algorithms and 3D dose distributions, understanding TAR remains important for fundamental dosimetry knowledge and for verifying complex treatment plans.
Comparing TAR with Other Dosimetry Methods
Let's explore how Tissue-Air Ratio (TAR) compares with other dosimetry methods like Percentage Depth Dose (PDD) and Tissue Phantom Ratio (TPR):
1. Percentage Depth Dose (PDD)
- Definition: PDD is the percentage of the dose at a specific depth compared to the dose at a reference depth, typically the depth of maximum dose (Dmax).
- Equation:
PDD=(D(z)Dmax)×100%\text{PDD} = \left( \frac{D(z)}{D_{\text{max}}} \right) \times 100\%
- Key Points:
- Depth Dependency: PDD decreases with increasing depth due to attenuation.
- Field Size & SSD: PDD values change with field size and Source to Surface Distance (SSD). Larger field sizes and SSDs increase the PDD.
2. Tissue Phantom Ratio (TPR)
- Definition: TPR is the ratio of the dose at a specific depth in tissue to the dose at a reference depth in the same medium (usually at 5 cm or 10 cm depth).
- Equation:
-
PDD=(D(z)/Dmax)×100%
- Key Points:
- Field Size Independence: Unlike TAR, TPR is less affected by field size and SSD.
- Energy Dependence: Higher energy beams result in higher TPR values due to deeper penetration.
Comparison of TAR, PDD, and TPR
|
Parameter |
TAR |
PDD |
TPR |
|
Reference Medium |
Air |
Water |
Water |
|
Depth Dependence |
Yes |
Yes |
Yes |
|
Field Size Effect |
Significant |
Significant |
Less significant |
|
Energy Dependence |
Yes |
Yes |
Yes |
|
Typical Use |
Traditional dosimetry |
Clinical dosimetry |
Modern TPS calculations |
Choosing the Right Method
- TAR: Useful for specific historical dosimetry calculations and for understanding basic principles of radiation attenuation.
- PDD: Commonly used in clinical settings for treatment planning involving external beam radiotherapy.
- TPR: Preferred in modern treatment planning systems due to its stability across different field sizes and SSDs.
Practical Applications
- TAR: Suitable for manual dose calculations in historical contexts or educational purposes.
- PDD & TPR: More commonly used in contemporary clinical dosimetry and treatment planning.